Mobile Menu
- About Us
- Research
- Education
- Policy & Data
- News
- Resources
- Giving
A low-glycemic index (low-GI) diet can be delicious, budget friendly and easy to make. This was the key message at the University of Toronto’s second annual culinary medicine event, held at George Brown College last week.
The event, organized by the Joannah & Brian Lawson Centre for Child Nutrition at U of T’s Temerty Faculty of Medicine, provided clinicians with practical knowledge and tips to share with patients on how to incorporate the low-GI diet into their lives.
“As physicians, part of being able to communicate about food, diet and healthy lifestyles to our patients is to learn about these things and model these behaviours,” says John Sievenpiper, professor of nutritional sciences at Temerty Medicine and chair of the event.
“Culinary medicine gives physicians and other health care professionals the opportunity to interact with the material directly — to see, smell, taste and touch the food — so that they can better communicate about nutrition to their patients. It helps them have a richer discussion to get the buy-in for behaviour change.”
More than 60 physicians and health-care professionals attended the U of T-accredited continuing professional education event, which included presentations, a cooking demonstration and a grocery shopping simulation, in the context of optimizing diabetes prevention and care through low-GI diets.
The low-GI diet emphasizes foods that do not cause spikes in blood sugar, and studies have shown that it can reduce the risk of developing type 2 diabetes and help manage the disease. Diabetes Canada recommends a low-GI diet to help control blood sugar levels.
This year’s event began with a presentation from the two researchers who developed the diet in the 1980s at U of T: University Professor David Jenkins and Professor Emeritus Thomas Wolever. They discussed how the diet was developed and incorporated into care guidelines, as well as the scientific evidence supporting the diet to prevent and manage type 2 diabetes.
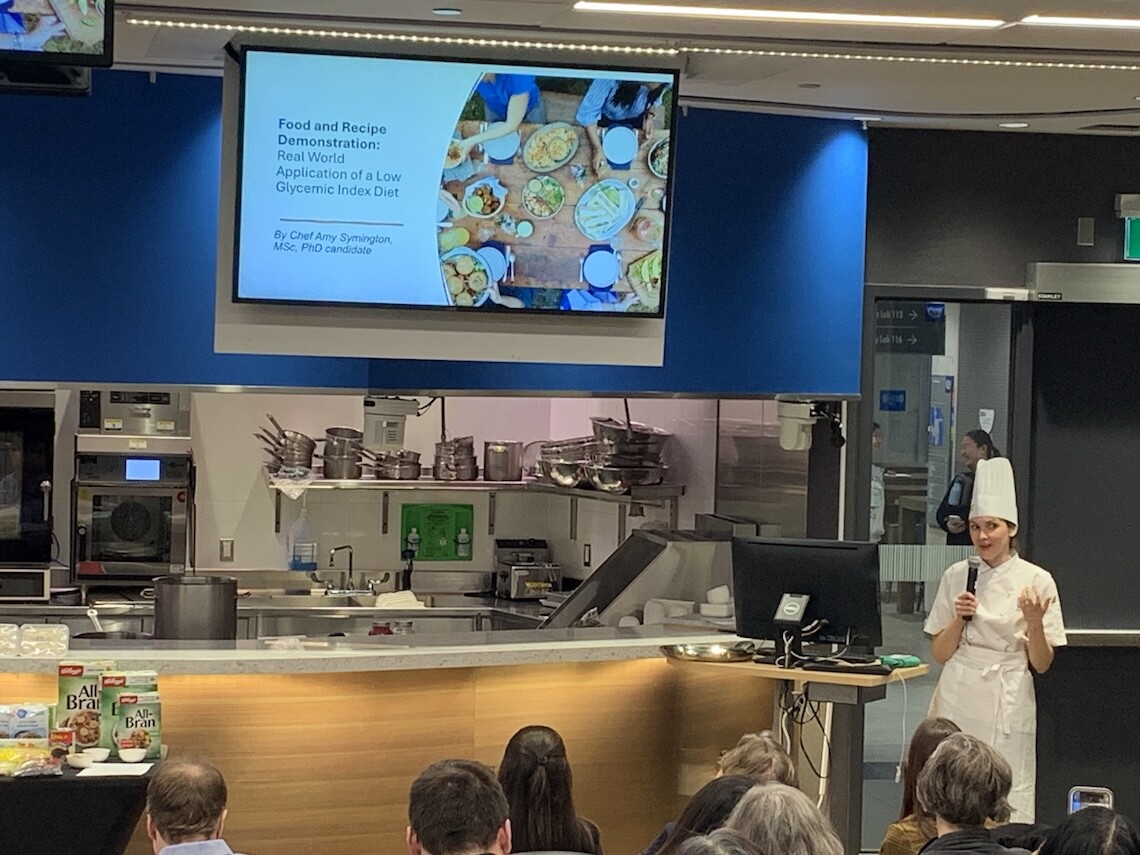
Amy Symington, a PhD candidate in nutritional sciences at U of T who runs culinary nutrition programming at the not-for-profit cancer organization Gilda’s Toronto, then applied this knowledge in a cooking demonstration and food tasting of low-GI recipes. She discussed cooking techniques that keep the glycemic index of certain foods low, such as cooking pasta al dente rather than soft, cooling foods after cooking and avoiding overly ripe fruits.
A highlight of the event was an opportunity to sample low-GI snacks, including oat and seed crackers with romesco dipping sauce, and mixed berry oat muffins. Symington also demonstrated three recipes: vanilla chai chia seed pudding and parfait, pasta with silken tofu and cannellini bean bechamel sauce, and tempeh chorizo tacos.
“Clinicians should talk to their patients about food choices that can improve diet, but if these foods aren’t practical, tasty, accessible, cost-effective, seasonal and culturally appropriate, people won’t eat them and they won’t make any difference in overall health,” says Symington.
“I hope that physicians, who are often on the front line of these discussions, will take back some simple tips and techniques, examples and resources that they can then provide to their patients.”
Andrea Glenn, assistant professor of nutrition at New York University, presented a grocery shopping simulation to teach clinicians where low-GI foods can be found and what to look for.
The event concluded with Laura Chiavaroli, assistant professor of nutritional sciences at U of T, who discussed digital tools to help patients stick to a low-GI diet, including an app she is co-designing in partnership with Diabetes Canada that helps patients determine which foods fit within the diet.
“This event was particularly exciting because it provided clinicians not only with knowledge but also tools and resources to help their patients make change. It translated the knowledge into practical demonstrations,” says Sievenpiper.
“Professors Jenkins and Wolever laid the foundation for this diet by providing the evidence and incorporating in into dietary guidelines. Now a new generation of researchers is translating this evidence into practical tools to help physicians counsel patients on how they can make change.”